Opioid dependence develops through a series of brain responses that influence motivation, reward, and emotional regulation. Dopamine plays a central role in this process, which is why cravings can feel strong even when someone wants to stop using opioids.
This article explains how dopamine functions, how opioids affect the brain, and why these changes shape cravings and daily decision‑making.
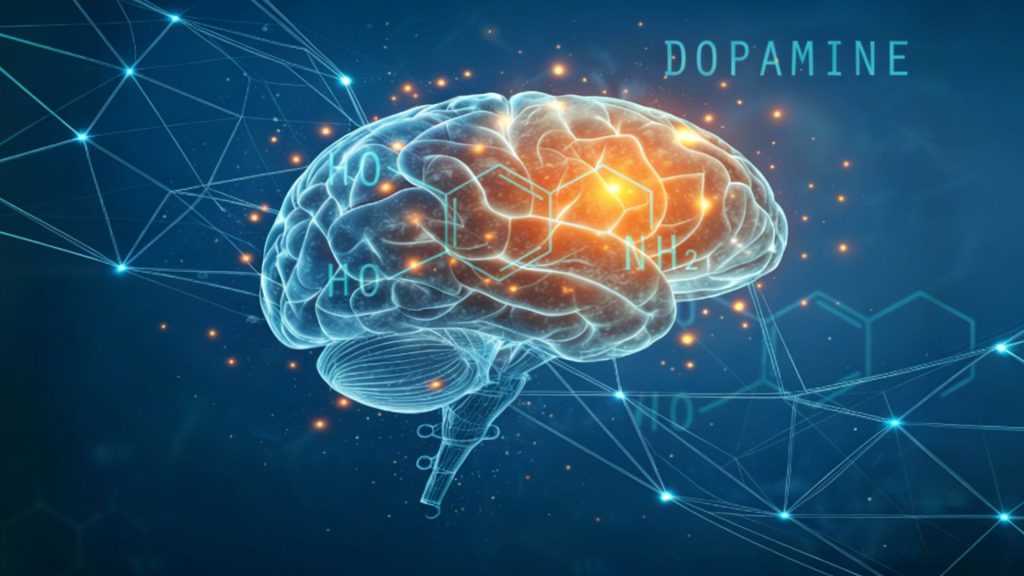
How Dopamine Functions
Dopamine acts as a chemical messenger that supports reward learning, emotional responses, and decision patterns. It helps the brain register experiences as positive or reinforcing. Eating, connecting with others, and completing tasks can release moderate amounts of this reward‑related chemical, which supports motivation and daily functioning.
Opioid use disorder disrupts these reward pathways and pushes the nervous system toward addiction. When these substances enter the system, they trigger a rapid surge of the reward signal. The system begins linking use with strong relief and comfort, and these associations strengthen quickly, making the drug feel more compelling than natural rewards.
Activity in these pathways becomes tied to the expectation of continued use. Treatment for opioid addiction helps interrupt these patterns as the brain adjusts to steadier chemical activity and begins reducing reward‑seeking linked to past use.
How Opioids Influence Dopamine Release
Opioids activate receptors in various parts of the brain, including areas responsible for reward and stress responses. This activation reduces pain signals and produces a strong sense of relief. The surge of dopamine that follows reinforces the behavior, teaching the brain to repeat it.
As exposure continues, the system adapts. Natural reward signaling becomes less responsive, while the artificially heightened surge from the substance remains much stronger. Everyday activities that once felt enjoyable no longer create the same effect. This imbalance strengthens the urge to keep using, because the system learns that the substance provides the most reliable path to relief.
These changes can appear early and may continue to influence behavior long after the last use. When these pathways shift, urges become tied to specific cues, routines, environments, and emotional states.
Why Dopamine Imbalance Creates Cravings
Urges often feel sudden, intense, or difficult to control. These associations develop through learned patterns, not immediate reward cycles. Once those links form, familiar cues can trigger internal reactions even during periods of abstinence, creating a sense of pull without any conscious thought.
Reduced natural signal production contributes to discomfort, restlessness, fatigue, or difficulty concentrating. The absence of natural reward activity can make urges feel more urgent because the system expects the substance to fill the gap. The cycle becomes self‑reinforcing: the substance triggers a strong surge, the brain adapts, natural signaling weakens, and urges grow stronger.
Stress can also influence this cycle. During difficult moments, the brain responds to tension by activating conditioned responses associated with past use. This reaction develops from repeated associations, creating automatic urges that arise even without conscious intent.

Dopamine, Withdrawal Symptoms, and Emotional Distress
Withdrawal symptoms reflect the brain’s adjustment period once opioid use stops. As dopamine pathways stabilize, people often feel the effects across mood, sleep, motivation, and physical comfort. Low dopamine levels may contribute to irritability, sadness, and difficulty experiencing pleasure.
These experiences are common during early abstinence. The brain is working to restore balance, which takes time. While cravings can feel overwhelming during this phase, they are part of the neurological repair process. Understanding this connection reduces fear and encourages people to stay engaged with support systems.
Environmental cues and emotional memories can also reactivate craving pathways during withdrawal. The brain remembers where relief once came from and responds automatically. These patterns decrease as the reward system recovers, especially when reinforced with new routines and coping skills.
How Treatment Supports Dopamine Stabilization
Treatment settings focus on stabilizing brain chemistry while teaching healthier responses to cravings. Medications used in opioid treatment programs, such as methadone, buprenorphine, and naltrexone, can reduce withdrawal symptoms and help balance dopamine signaling. This gives the system space to regulate itself without extreme highs or lows.
Therapy also plays an important role. People learn how craving cues form and how to respond without acting on them, which strengthens relapse prevention skills grounded in awareness and routine. Skills that support emotional regulation, stress tolerance, and daily functioning help reduce the intensity of dopamine‑driven urges. The reward system begins to respond more naturally to everyday life activities.
A supportive environment strengthens this process. Healthy routines, steady sleep, social connection, and positive reinforcement help rebuild the brain’s ability to release dopamine in balanced ways. These changes do not happen instantly, but they create a foundation for long‑term wellness.
Final Thoughts from Blueview Recovery
Dopamine plays a central role in opioid dependence, especially in the development of urges and reward‑seeking patterns. When exposure alters dopamine activity, the brain becomes conditioned to expect strong relief from the substance, making urges feel persistent and difficult to manage.
At Blueview Recovery, our team understands how these neurological shifts influence opioid addiction. Our opioid addiction rehab program in Philadelphia, PA, includes evidence‑based therapies designed to address these reward‑driven patterns and help people regain steadier functioning.